Client Profile
The client is a 30-year old RCM company dealing in medical reimbursement management for hospitals and providers in the West Coast. Its offering includes medical billing services and revenue cycle solutions including billing, coding, credentialing and consultation services.
The Backstory
For 3 decades, it depended largely on manual processes to fuel RCM operations. The gradual surge in work started challenging the efficiency of the workforce. As it was already overstretched, automation of repetitive and time-consuming tasks emerged as the prudent choice.
Challenge
Payment process
Claims status check process
Among the processes, insurance claim status check and payment posting were draining resources significantly.
The payment processing team fetches claims information from the front office web portal and generates the report. Claims with a status other than ‘Accepted’ are followed-up with the insurer and the details are communicated to the patient. This is repeated frequently until the claim is closed.
Payment posting process
In the ePosting process, payers send an ERA (electronic remittance advice) towards the payment of each claim. The payment poster posts these into the respective patient accounts in the provider application, against that particular claim. The process is rule-based and indicates the cut-off levels for adjustments, write-offs, refund, etc. It’s repeated for multiple providers.
By their nature, these are simple and straight-forward but also tedious and error-prone – perfect candidates for automation.
The solution
Nalashaa’s RPA team built a robot tailored to the specific requirements of the two processes to cut down on the manual tasks, and boost efficiency and accuracy.
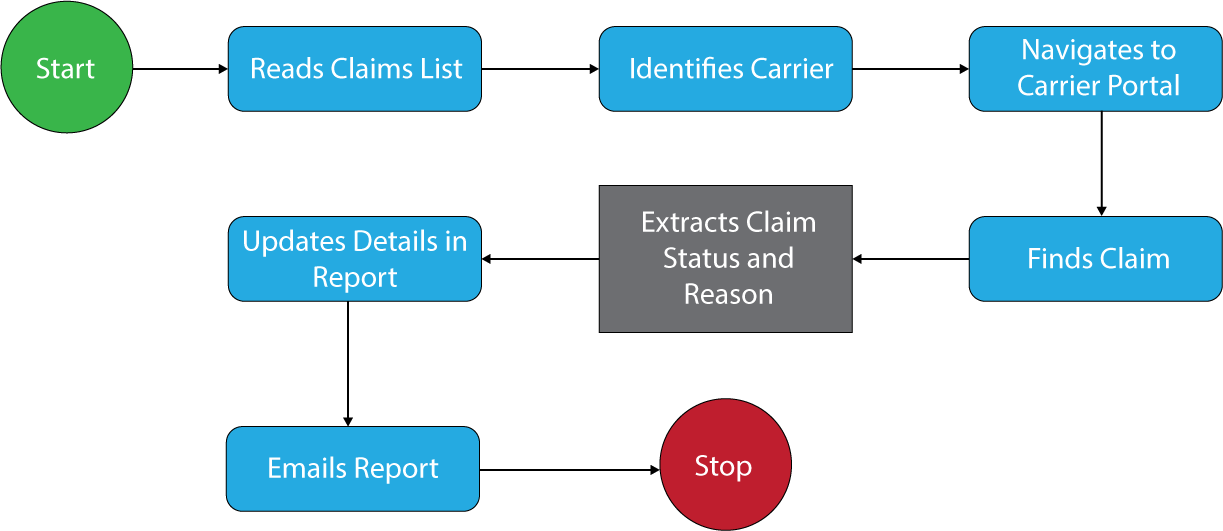
Read claims reports: The bot reads the report containing the claim information, identifies the Carrier, and logs into the respective carrier portal.
Search the claims: Inside the carrier portal, it searches for the claim using the claim number and date and extracts the claim status (Accepted, Deferred, Denied, or Close) and details.
Email claim status: It then sends a report of the claim details to the client to prompt actions.
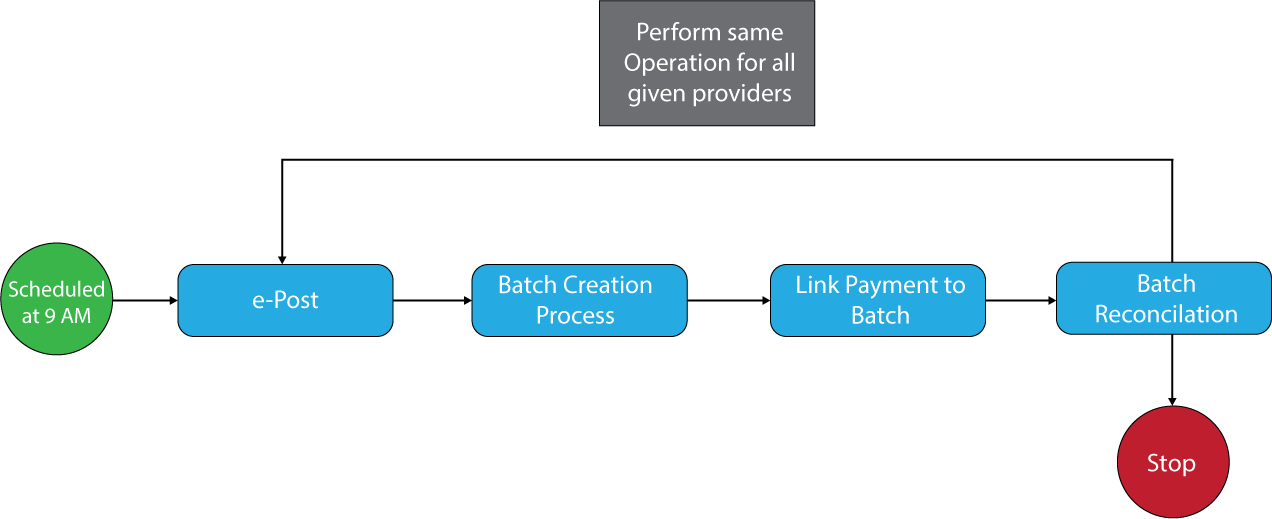
Authenticating provider application and accessing unposted claims: Bot authenticates provider application, identifies the ‘Unposted’ claims and, accesses the ERA. It adds the columns of total posted, batch number and total, and comments to the ERA spreadsheet that contains details such as EFT date, carrier name, etc.
E-Posting Process: For each record in the spreadsheet, the bot selects the ERA file using the file number and E-posts it.
Batch creation: The bot then creates a new payment batch and for each record in the spreadsheet, it retrieves the batch number and links the payment to the batch.
Update Deposit log and Query Log: Files with posted amount are moved to the deposit log (Excel report), and those with unposted (due to errors while posting) amount are moved to the Query log.
Batch Reconciliation: Once all the files are posted, the batch total is reconciled with the actual posted and exception email are triggered for the discrepancies.
Task notification: The bot sends a status email to the mailer and the team as specified in the configuration file. The same process is repeated for all the given providers.
- Reduced Headcount – Reduced administrative work
- Faster Processing and Higher efficiency - Increased Customer Satisfaction
- Data Validation – Fewer errors
- Automation of repetitive tasks - Staff Satisfaction, allowing the person to perform high-value work.
Report Card
Claims status check
| Pre RPA | Post RPA | |
|---|---|---|
| Transactions per day | 600 | 1000 |
| Accuracy rate | 67% | 98% |
| Headcount | 5 | 1 |
| Avg. time for each transaction | 5 minutes | 1.5 minutes |
Payment posting process
| Pre RPA | Post RPA | |
|---|---|---|
| Transactions per day | 400 | 900 |
| Accuracy rate | 71% | 97.5% |
| Headcount | 4 | 1 |
| Avg. time for each transaction | 5 minutes | 2 minutes |
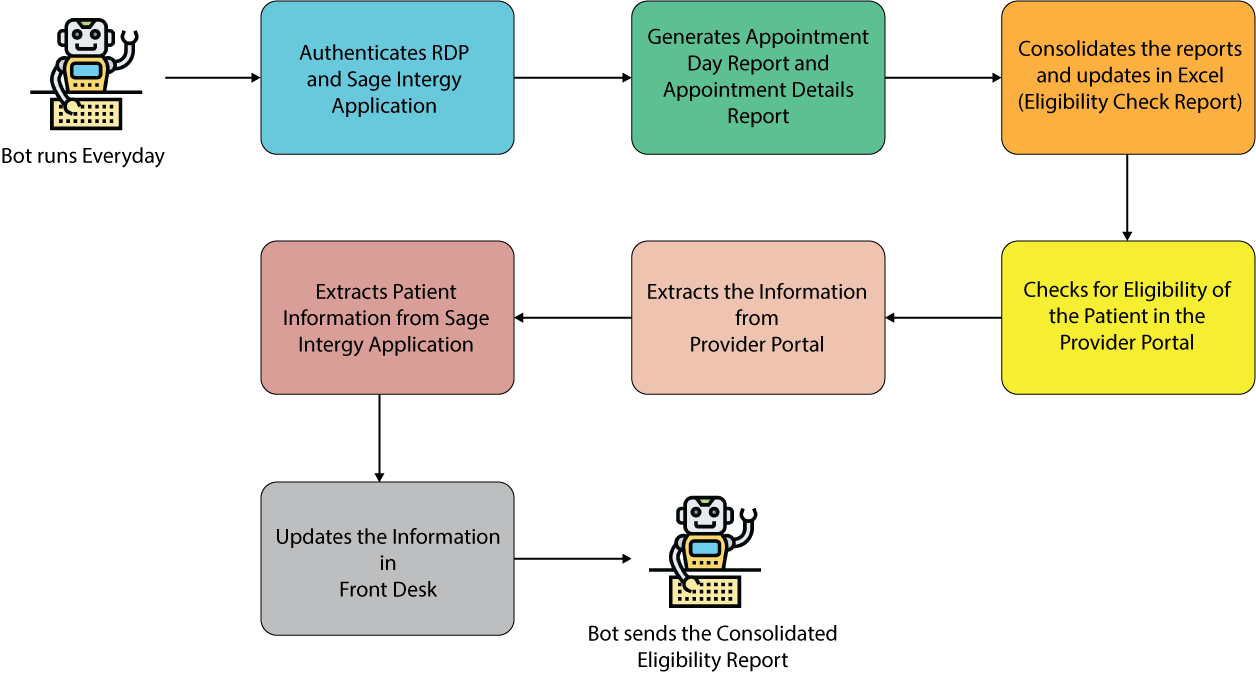
Process Flow Diagram
Technology Stack
- UiPath
- eClinicalWorks – Web Portal
- Front office web portal
Speak to our Experts!
Countless businesses around the world and across industries have gained substantially from smart RPA implementations. Over the last decade, we have enabled our clients to transform their business by tapping their true potential with RPA. We can help you do that too!