Healthcare has been acquainted with AI for longer than most industries realize.
The earliest wave focused on prediction and classification. Models flagged risk, predicted outcomes, and categorized images. These systems were powerful but narrow. They answered questions but never acted on the answers.
The next wave brought generative AI. Large language models could summarize notes, draft content, and converse in natural language. This definitely reduced clerical work, but the workflow still depended on humans to decide what to do next. That’s actually a problem during mission critical tasks.
That’s when Agentic AI introduced a different capability.
Instead of stopping at insight or content generation, agentic systems are designed to act toward a goal. They can perceive what is happening, plan steps, execute actions across systems, observe the result, and adapt their behavior over time.
The critical distinction is not intelligence. It is “agency”.
What People Mean by Agentic AI in Healthcare?
When healthcare leaders talk about agentic AI, they are not referring to another dashboard, chatbot, or predictive model. They are describing a shift in how work actually gets done. Agentic AI changes AI’s role from advising humans to carrying out coordinated actions under human oversight.
Across the BCG analysis, five traits consistently define what makes an AI system “agentic” in a healthcare context.
First, agentic systems observe continuously.
They do not rely on static snapshots of data. Instead, they ingest live signals from electronic health records, wearables, imaging systems, claims data, genomics, operational workflows, and patient behavior. This constant observation allows the system to maintain situational awareness as conditions evolve, rather than reacting after the fact.
Second, they plan across steps.
Traditional AI answers questions such as “What is the risk?” or “What does the data show?” Agentic AI goes further. It determines what should happen next, in what sequence, and under which conditions. The focus shifts from insight generation to decision orchestration.
Third, they act autonomously.
Once a plan is formed, agentic systems can execute tasks without waiting for manual handoffs. This may include submitting prior authorizations, scheduling care, triggering diagnostics, routing cases, generating clinical documentation, or initiating patient outreach. Action is the default, not the exception.
Fourth, they adapt based on outcomes.
If an action does not produce the expected result, the system does not stop and wait. It adjusts the plan, retries through an alternative path, or escalates when thresholds are met. This feedback loop is critical to moving from automation to autonomy.
Finally, they remain human-supervised.
Agentic AI in healthcare is not about removing people from the loop. Clinicians and staff approve, override, audit, and set boundaries. Control does not disappear; it becomes more strategic. Trust is built through transparency, explainability, and governance.
Use Cases of Agentic AI in Healthcare
I know a lot of this may sound familiar. Many teams are already talking about agentic AI, and you may have seen similar ideas before. That is completely expected.
Where this becomes real is not in the concepts, but in where you choose to apply them.
We can absolutely help you implement agentic AI in your environment, but the starting point matters. The most effective way forward is to anchor it to a specific workflow where autonomy can genuinely improve outcomes.
You can choose from the use cases we have already outlined, such as care coordination, prior authorizations, claims operations, or post-discharge follow-up. If none of those reflect your current priorities, that is fine too. Many organizations have unique workflows shaped by their systems, patient populations, and operational constraints. Let us know your unique requirements.
1. Clinical Decision Support That Actually Acts
In most hospitals, decision support has not failed because models are weak. It has failed because action still depends on humans stitching context together under time pressure.
What is changing is not the alert itself, but what happens after risk is detected. Agentic systems are being used as orchestration layers that sit across the EHR, labs, medication history, and protocols. Instead of pushing generic alerts, they assemble the case context first and surface only the signals that are likely to require action.
In high acuity environments, this shows up as continuous monitoring of vitals and labs with prioritized escalation. The system pulls recent results, active medications, contraindications, and guideline relevant criteria, then prepares the likely next steps before the clinician is interrupted. That could mean drafting orders, recommending a care bundle, or highlighting missing tests that would otherwise be discovered late. The workflow is designed to reduce false noise, shorten time to treatment, and prevent the common failure mode where correct alerts are ignored because acting on them is too time consuming.
This approach fits early because it augments clinical work rather than trying to replace it. The clinician still decides, but they do not have to reconstruct the situation from scratch.
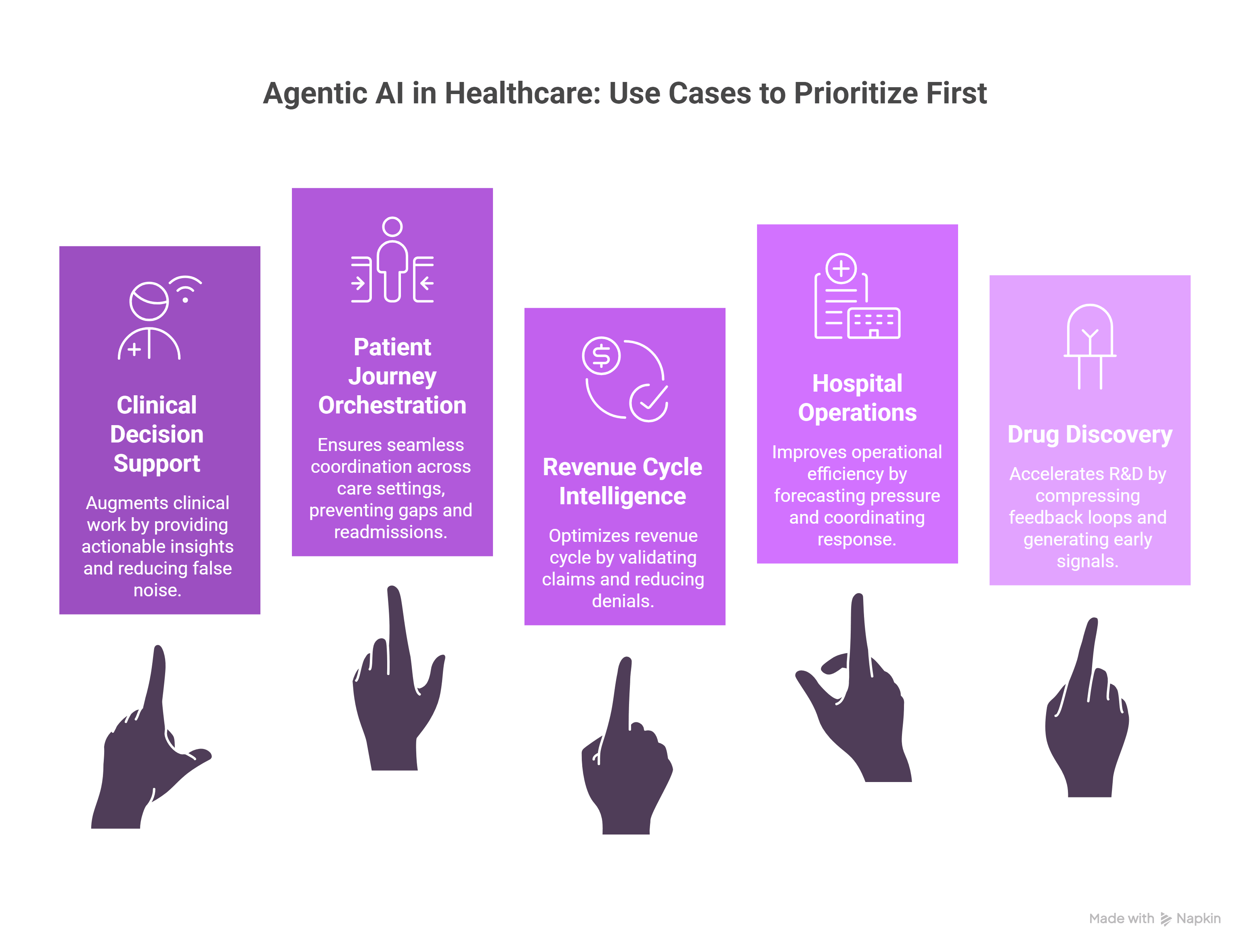
2. Patient Journey Orchestration Across Care Settings
Patient journeys break when coordination does not hold across settings. Outpatient follow ups, post discharge plans, home monitoring, labs, referrals, and patient communication often sit in separate systems, and care teams do not find gaps until they become escalations.
Agentic systems are being used to keep these journeys intact through persistent orchestration. They track expected milestones, check whether tasks are completed, monitor vitals or symptom data where available, and intervene when something stalls. Instead of relying on manual reminders and patient memory, the system can reschedule missed follow ups, trigger outreach when remote data stops flowing, and escalate early signals to the right team.
The practical difference is that monitoring is tied to action. Not more dashboards, not more alerts, but a closed loop that detects drift and initiates the next step. This is why these deployments are showing traction in chronic care programs and post discharge pathways where small delays become readmissions.
3. Revenue Cycle and Claims Intelligence
Revenue cycle work breaks because most systems detect issues late. Denials arrive weeks after submission, missing documentation is discovered after the claim is already stuck, and staff spend time chasing portal status rather than preventing failure.
Agentic AI is being applied as a coordinating layer that follows the claim end to end. It validates coding and documentation before submission, applies payer specific rules consistently, and flags gaps while they are still fixable. When denials occur, the workflow does not restart with manual investigation. The system pulls the relevant evidence, drafts the appeal, routes it for review, and tracks submission and response.
This is a low risk entry point because it sits in administrative workflows with clear policies, high volume, and measurable cycle time impact. The teams getting value here are moving toward touchless handling for routine claims and reserving human effort for true exceptions.
4. Hospital Operations and Capacity Optimization
Operations teams rarely struggle because they cannot see what is happening. They struggle because they see it too late. Bed pressure, staffing shortages, delayed discharges, and ED congestion are often visible only after the floor is already strained.
Agentic systems are being used to forecast pressure and coordinate response across systems rather than reporting yesterday’s performance. They ingest admission patterns, length of stay signals, discharge readiness indicators, and operational constraints, then trigger earlier actions such as discharge checklist initiation, staffing adjustments, or bed turnover coordination. The value comes from orchestration that links prediction to execution rather than leaving teams to interpret dashboards and act manually.
These deployments tend to start in areas where decisions are repeatable and rules are well defined, such as discharge planning, staffing optimization, and bed management workflows.
5. Drug Discovery and Clinical Research Acceleration
R and D slows down because feedback loops are sequential. Experiments run, results are reviewed, hypotheses are updated, literature is incorporated, and trials are adjusted, often with long delays between each step.
Agentic AI is being used to compress these loops by running work in parallel. Systems continuously ingest new evidence, generate and test hypotheses in silico, update models as data arrives, and surface early signals of toxicity or low efficacy before late stage costs accumulate. Trial operations can also be coordinated more tightly through automated eligibility screening, recruitment support, and ongoing monitoring of protocol adherence.
The results that matter are reduced iteration time and earlier quality signals. The objective is not replacing scientific judgment. It is removing coordination and search overhead so teams can run more cycles of learning in the same calendar time.
Steps to Implement Agent AI in Healthcare
You have probably heard a lot about agentic AI in healthcare by now.
What agentic AI in healthcare is?
How it differs from traditional AI?
The features of agentic AI in healthcare and why it is being positioned as the next operating model for hospitals, payers, and life sciences organizations.
What most people do not tell you is how to implement agentic AI in healthcare.
Here are some guidelines that will definitely help you find your path:
Phase 1: Choose the Right Entry Point (Weeks 1–4)
Start by selecting one workflow where work already feels broken
- Span multiple systems (EHR, payer portals, scheduling, email)
- Require constant follow-ups
- Depend on people remembering the “next step”
- Have clear delays or backlogs
Here are some common starting points
- Prior authorizations
- Post-discharge follow-ups
- Claims appeals
- Care coordination workflows
- Scheduling and patient outreach
Here is what not to do
- Do not start with chatbots
- Do not automate a single step
- Do not start with high-risk clinical decisions
Phase 2: Define the Outcome and Guardrails (Weeks 3–6)
Before touching any AI tools, define:
- What success looks like
- Where AI is allowed to act
- Where humans must stay in control
Example goals
- Reduce authorization turnaround from 7 days to 3
- Increase post-discharge follow-up completion to 85%
- Cut claims resubmissions by 30%
Now you need to set autonomy boundaries
- What the agent can do on its own
- What requires human approval
- What the agent can only recommend
Phase 3: Design the Orchestration Layer (Weeks 6–10)
Instead of building one big “smart agent,” design a coordinator.
This orchestration layer:
- Tracks workflow status
- Assigns tasks to agents
- Handles delays, retries, and escalations
- Knows when to bring in a human
Think of it as:
“The system that makes sure work keeps moving even when something changes.”

